In the latest episode of our Poison Ed podcast, NNEPC Vermont educator Gayle Finkelstein sits down with Dr. Thomas Delaney and Dr. Rebecca Bell of the University of Vermont’s Larner College of Medicine to talk about trends in self-poisoning among Vermont youth. Listen below.
TRANSCRIPT
Gayle Finkelstein: Welcome to Poison Ed. This is Gayle Finkelstein, Vermont educator from the Northern New England Poison Center.
Today we are going to talk about suicide in Vermont, specifically focusing on self-poisoning suicide attempts. I’m joined by two guest speakers: Dr. Thomas Delaney, assistant professor at the University of Vermont’s Larner College of Medicine, Department of Pediatrics; and Dr. Rebecca Bell, pediatric critical care physician and assistant professor in the Department of Pediatrics at the Larner College of Medicine at the University of Vermont. Thank you both for joining us today.
I would like to start off helping our listeners understand the relationship between suicide attempts and poisons.
Using data from the National Poison Data System, which reports information from all 55 poison control centers across the country, researchers found more than 1.6 million children and young adults aged 10 to 24 years attempted suicide by poisoning between 2000 and 2018. The number of children and young adults who have attempted suicide by poisoning has increased in the United States over the past several years. There was a significant increase in the rate of attempts between 2011 and 2018 that was driven predominantly by girls and young women. A total of 71% of all cases reported in a recent study published in the Journal of Pediatrics involved females. While the study’s data cannot point to a specific reason behind the increase in self-poisoning, it was noted that social media and internet use have increased significantly during the same period.
The Northern New England poison Center continues to see high numbers of calls from health care providers seeking management consultation, most often related to self-harm attempts. We are seeing females more than males attempting suicide. For females, the 13- to 19-year-old age category had the highest number of cases, and for males it was 20- to 39-year-olds. Suspected suicide attempt remains a significant concern, accounting for 14% of exposures this past year from Vermont.
Dr. Delaney, what recent trends in the Vermont data and U.S. suicide deaths are you seeing?
Dr. Thomas Delaney: Well, unfortunately, Vermont suicide death rates have been trending in the wrong direction for a long time, with over a 30% increase in the rates since 1999. We use rates of people per 100,000 in order to compare across different states and between states and the U.S. as a whole. Nationally, suicide death rates have also been increasing, and the U.S. in recent years has basically been catching up with Vermont’s already higher rates. The trends that we’re seeing are pretty much holding for middle-aged and older people as well as for younger people.
GF: Why are the suicide rates in Vermont so high?
TD: Well that’s a huge question, and it’s really important to distinguish between suicide attempts and suicide deaths, and especially important to note that when we’re talking about young people who attempt to take their lives, they have about 25 suicide attempts for every death and that’s a really different picture than what we see for middle-aged and older folks, who have fewer attempts but are more likely to die from their attempts.
We also have to acknowledge that every person who dies by suicide has their own circumstances, and the causes of the suicide death are often not clear and very complicated. So what’s true for a population of people, which is really what I’m talking about, may not be true for the individuals from the population. And when we think about population-level risk factors that are higher in Vermont:
- We have an older population—so, we’re one of the oldest states in the U.S. in terms of our mean and median ages
- We have a high rate of military participation—so there is this effect where nationally veterans die by suicide at a rate about twice the rest of the adult population, and we do have a lot of veterans in our state
- We have high rates of binge drinking, which is also correlated with suicide deaths
- We are also a very white state, and interestingly, when we think about different racial groups and suicide risk, white, Caucasian people actually have higher rates than some ethnic minorities and racial groups have.
So I think that’s pretty much the big population-level risk factors. The one I left off—and that is really notable—is the high rates of firearm ownership, as well. So there is a correlation between states having higher rates and easier access to firearms and having higher suicide death rates.
GF: When you identify the specific groups that may be at higher risk, is there one specific group that stands out?
TD: Well when we look at people who actually die by suicide, if you look retrospectively at what they were dealing with, you do see that people who were struggling with serious mental illness and experiencing chronic life stressors are at higher risk for dying by suicide. And in Vermont we see that veterans, as I already mentioned, are about twice as likely to die by suicide than are the rest of the adult population.
In general when we’re thinking about suicide in middle-aged and older people, a lot of times we’re talking about males. So there are, for those ages it’s about four males who die by suicide for every female, and many of those people who die actually fall into the other categories—for example, of struggling with substance abuse, being veterans, rural, social isolation, things like that.
We know that when we’re thinking about younger people, LGBTQ young people in Vermont—and this is based on the Vermont Youth Risk Behavior Survey—they’re about three times more likely to have felt sad or hopeless every day for the past two weeks, and that’s a marker for major depressive disorder. And the same young people are about four times more likely to have hurt themselves on purpose compared to non-LGBTQ young people. LGBTQ young people in Vermont are also about four times more likely to have made a suicide plan in the past year and four and a half times more likely to have made an actual suicide attempt.
Also thinking about young people and increased risks, we know that students of color are about 50% more likely to have made a suicide plan in the past year, as well as being more than 50% more likely to have made a suicide attempt. We also know that young people and indeed people of all ages with a history of trauma are at elevated risk for suicide deaths and attempts.
GF: Dr. Bell, what is your experience as a physician regarding youth and deliberate self-poisoning?
Dr. Rebecca Bell: So I work in the Pediatric Intensive Care Unit, so my patients, who are in the Pediatric ICU from a self-poisoning are either critically ill, so experiencing really severe symptoms or are at high risk of experiencing severe symptoms or even death.
What I’ve noticed with my patients is that there’s quite a range. So, many youth have a history of a serious mental health illness like depression or anxiety, but some do not have that history. All of them have some sort of trigger that lead to their self-poisonings, and what my patients generally tell me once they feel better and they can talk about their experience is that maybe they’ve been feeling down or maybe they haven’t been feeling down, but regardless they get in a fight with their parent or friend or something happens at school or something happens on social media, and they take medicines, and oftentimes, afterwards, they tell someone. So they tell a parent, or even more often they tell a friend about the self-poisoning. And what I’ve noticed in Vermont among my patients is that young people are really good at getting help for their friends. So oftentimes the young person will take medicine, then after some time period will text a friend and say what they’ve done, and that friend will immediately tell a parent who then gets help. So that I have found to be really important.
And I think that, you know, young people, every young person is at risk for a self-poisoning, because young people are more impulsive than adults and they engage in more impulsive behaviors, and things that happen in their life that may seem a little bit trivial once you’re older can seem really, really important and young people can be really distressed. So again this breakup of a relationship, or an event at school where someone gets bullied, those can be really, really distressing for young people, and young people are at risk for that happening. So we really want to encourage all families to create safe environments in the home, so that when they have one of these events that they don’t have access to medications are other things that could hurt them.
GF: I had mentioned earlier about a recent study looking at national suicide and self-poisoning, especially regarding sex- and age-specific suicide attempts by self-poisoning. This report indicates that the first episode of deliberate self-poisoning is a strong predictor of subsequent suicide and premature death. While almost all individuals survive their first hospital presentation for self-poisoning, the risk of subsequent suicide was more than fortyfold higher in these patients than among population-based controls.
The highest number of cases nationally poison centers received was in the 13- to 18-year-old age category. For children under 19 years of age the annual suicide attempts by self-poisoning doubled from 2000 to 2018. Serious outcomes also increased 235%.
Overall, suicide attempt rates are increasing in Vermont. The Northern New England Poison Center reported 5,459 suicide attempt cases between 2009 and 2018, with 23 of these resulting in death.
Dr. Delaney, why is having Vermont self-poisoning data is so important?
TD: I think there’s a couple reasons why this is really important data for us to look at. So, Vermont can really differ from other parts of the country and indeed from other parts of New England and the Northeast. We already talked about how we’re a little bit different in terms of owning firearms and some other characteristics as well.
So having these data is really a way of informing and maybe even developing new prevention programs. So we can think about community education. One thing that I’m really interested in is provider education. So how do you support health care, mental health care providers to maybe do screenings? Or how to effectively intervene or make effective referrals to other types of providers when there has been an episode of intentional self-poisoning. And ideally we’d want to use the data and different types of public health approaches to get upstream and actually be preventing the suicide attempts in the first place.
It’s probably also really important that we raise awareness among community members and families and caregivers because ultimately they’re going to be doing a lot of the actual sort of safety steps and a lot of the initial responses when there is a risk of somebody engaging in self-poisoning.
GF: Dr. Delaney, what is the difference between risk factors and warning signs?
TD: Right, so I think of risk factors as being things that are more static and longer term. So a risk factor could be something like struggling with mental illness, where you were previously diagnosed and it may be better over time or a little worse over time, but it’s just something that’s present there for you.
I think of warning size signs as being much more in the moment, and they might be represented as a specific behavior or specific language. So a sort of classic warning sign is people who already have risk factors present may give away their possessions, for example, or they may verbalize something like “I won’t be here next week” or “I won’t be around much longer.” I’d called those warning signs.
GF: OK, and Dr. Bell, what are the clinical impacts on young people who are hospitalized for poisoning suicide attempts?
RB: So we have a number of different treatment modalities we can use in the Pediatric ICU to help take care of youth who are critically ill from their self-poisoning. So we can support their breathing if needed, sometimes with a ventilator if necessary. We can support their heart, their blood pressure, we can treat arrhythmias, treat seizures, fix electrolyte abnormalities. We’ve had to put some young people on dialysis. So in the ICU we have a lot of ways to make young people better. Some medications have antidotes that we can give as well.
But these young people are really sick, sometimes for many days, and there’s always a risky period where we’re not sure if there’s going to be long-term effects, long-term effects on their organs. So it can be a pretty tense time in the ICU for the young person, for their family.
And then once they’ve recovered, they will all end up going to an inpatient psychiatric facility where they can get intensive psychiatric care. Then when they are discharged home there’s a plan made between the psychiatric facility, the pediatrician at home, the family and whatever other therapy and counseling they need when they go home to make a real, again, safe environment for the young person when they leave.
GF: OK, and Dr. Delaney, how is Vermont addressing this problem?
TD: Well Vermont’s really ramped up their efforts in recent years I would say. So as one example, the legislature is supporting the Department of Mental Health to do an initiative called Zero Suicide. So the Department of Mental Health is teaming with the Center for Health and Learning and the Vermont Suicide Prevention Center, and they’re working with the designated agency system that is responsible for a lot of the community-based mental health care in the state, and they’re doing things like doing a lot of workforce development—so training on suicide-specific treatment modalities. For example, there’s one called CAMS—collaborative assessment and management of suicidality. And there’s other aspects of Zero Suicide, as well.
And there’s a big focus on fixing some of the gaps in the system. So one of the gaps that we’ve heard about in the past in our state, and certainly in other places, is handoffs between people who show up in the emergency department who have suicidal ideation or suicide attempt and just then making sure that they actually wind up starting to get care once they’re out of the emergency department. Certainly making links between inpatient hospitalization and care once those people are discharged that Dr. Bell mentioned.
And a lot of education and outreach to mental health providers and community-based providers who weren’t necessarily getting a lot of the suicide prevention-specific sort of training and opportunities that now they’re getting a lot more of. And we know there’s some evidence that actually having those trainings makes the mental health care system and probably also health care providers be more effective in helping their patients.
GF: And Dr. Bell, what are things that all families should be doing in order to keep people from accessing poisons?
RB: Well we tell all families that they should keep medications truly inaccessible to young people, even adolescents. So that means locking up medications, it means when a young person is on a prescription medication that the parent should be the one who sort of controls that medication and gives the young person the medication, and that helps, one, prevent the young person from taking a bunch of that medication, and also makes sure that they’re actually getting it on time when they need it.
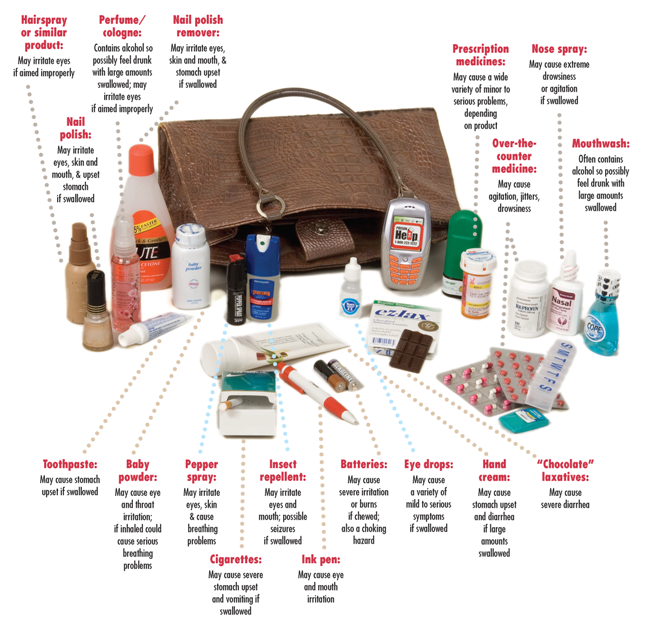
And one thing families oftentimes underestimate is how serious and dangerous over-the-counter medications can be. So, many of the patients that I see in my PICU are there and critically ill from over-the-counter medications. So we often don’t think of that as being potentially dangerous, but it can be. So even over-the counter-medications I would say try not to buy in bulk, and again, I would keep those inaccessible and have the young person ask for them and you can give it to them in a controlled manner. And the same thing with of course the parents’ prescription medication. So really all medications should be really inaccessible to the young person.
GF: How about in terms of health care providers, regarding intentional self-poisoning in young people—do you have any advice?
RB: Yeah, I would say all health care providers should really think about, when they’re prescribing a medication, about whether there’s a young person in the house. So I do see some patients who come in who have taken their parent’s medication, for instance, and so if you’re a health care provider, even if you’re treating adults, asking about children in the house is really important, so that if you’re prescribing something that can be dangerous in large quantities that you’re providing some counseling on how to keep that medication inaccessible to the young person. Oftentimes I see cases where, say, a health care provider is prescribing something to an adult or a young person that they’re going to try to see if it helps their symptoms, and then it doesn’t really work, and then you’ve got now this bottle of medications in the home. So I think following up on that, “Oh that medication didn’t work—why don’t you bring that in next time and I can discard that for you?” or the family can discard that. So not having a lot of medication sort of hanging around. And then I think counseling families, again, on keeping medications out of reach.
And I think it’s just really important for families to understand that adolescence is a difficult time and stressful things happen, and a lot of times I do see families who come in that are very surprised by the self-poisoning, and I just really want to emphasize that every young person is at risk for self-poisoning because things happen, stressful things happen, and when something’s accessible to them they may in an impulsive move use it. So remembering that really every adolescent is at risk.
GF: Well those are great points. The poison center also recommends keeping medicines up high and out of reach of children and teenagers, and to really remind parents to be mindful of all medications they keep in their house, and especially the old and expired medications should be disposed of safely, and if you are looking to find guidelines, you can either visit our website at the poison Center at nnepc.org, or also go to the Vermont health department’s website to see how you can properly dispose of your medications safely.
If children are prescribed any medication they need to be monitored like Dr. Bell said closely to ensure it’s being used correctly. Patients attempting suicide most often takes substances easily available to them like Dr. Bell had mentioned, especially over-the-counter medications and prescription medications. It’s also important to remember that many of the cases we see at our poison center and poison centers across the country involve multiple substances.
Do either of you have any other prevention strategies or resources you would like to share with our listeners?
TD: Yeah, I think just building off what Dr. Bell just mentioned, about adolescence being a tricky time for a lot of people, a piece of universal advice for parents and caregivers is to just check in with your kids. And that doesn’t mean necessarily prying—I have two teenage girls and I’m not allowed to pry into their lives at all—but even just checking in and saying “How are you doing?” or “How are things at school?” I think sometimes parents might be surprised by what they learn from doing that.
GF: And Dr. Bell, do you have anything else you want to share?
RB: No.
GF: OK, so our focus today has been on youth, but our poison center is also seeing an increase in patients attempting suicide in those over 60 years of age involving their own medicines. So some of these medications can be quite dangerous in overdose situations.
The Northern New England Poison Center is an integral part of the emergency medical care system and provides fast assistance and necessary assurance to residents and health care providers for Maine, New Hampshire and Vermont. In closing I would like to remind you that the poison center is available 24/7—it’s free and confidential—to help in poison emergencies or to just answer poison-related questions. You can reach the poison center toll-free at 1-800-222-1222, you can text POISON to 85511, or you can chat live at www.nnepc.org. The poison center is an important resource available to everyone and it’s right at your fingertips.
So I’d really like to, again, thank Dr. Bell and Dr. Delaney for joining us today and sharing their expertise. Thank you very much.
TD: Thank you.
RB: Thanks for having us.
GF: Thank you for listening to this episode of Poison Ed. If you or someone you know is in crisis, we encourage you to get support by calling the National Suicide Prevention Lifeline at 1-800-273-TALK, that’s 1-800-273-8255. You can also get support by text. Send the word HOME, that’s H-O-M-E to 741741 from anywhere in the United States, or text VT, for Vermont to the same number, 741741, for Vermont-specific resources. Thank you.

 One good way to clean out your medicine cabinet is to take your expired or unneeded medications to a take-back event. For several years, the DEA has been holding medication take-back events twice a year at locations across the country—typically a local police department. Visit the
One good way to clean out your medicine cabinet is to take your expired or unneeded medications to a take-back event. For several years, the DEA has been holding medication take-back events twice a year at locations across the country—typically a local police department. Visit the