We are pleased to announce the launch of Poison Center Pointers, a podcast brought to you by the specially trained professionals who answer your calls on the poison help line at the NNEPC.
What is it like working for a poison control center? What types of calls do we get? Get insights straight from the experts themselves while learning about ways you can avoid poisonings, and what to do in cases of possible poisoning.
Our first episode provides an introduction to poison centers and your local center, the NNEPC. Visit our podcast home page on Podbean to subscribe, or find Poison Center Pointers on Amazon Music, Apple Podcasts, Google Podcasts or Spotify.
TRANSCRIPT
Disclaimer: Poison Center Pointers is brought to you by the Northern New England Poison Center. This podcast is NOT to replace timely advice or recommendations. If you have an actual poisoning emergency, scenario or question, contact the Northern New England Poison Center by calling 1-800-222-1222, texting the word POISON to 85511, or chatting online at nnepc.org
Welcome to Poison Center Pointers, a podcast presented to you by the Northern New England Poison Center. ♪upbeat music♪
Chris: Hello to all our listeners, and welcome to the first ever episode of Poison Center Pointers, a podcast presented to you by the Northern New England Poison Center. My name is Chris, I am one of the specialists in poison information, and I am joined by two of my co-hosts and colleagues, Karlee and Carolyn. Thanks for being here, guys.
Karlee: Yeah, hi everybody!
Carolyn: Yeah, thanks for having us.
Chris: In this room we have a couple decades of experience here. A couple of those decades do come from Carolyn…
Carolyn: Thanks, Chris…
[laughter]
Chris: We decided to start a podcast here to share our knowledge and experience dealing with everyday situations we help manage at the poison center. Our goal is to keep the community safe by preventing a poisoning, but also making sure that you know what to do if a poisoning occurs. We’re hoping with the podcast we can provide some entertainment value along the way.
Carolyn: Maybe…
Karlee: We think we’re pretty funny!
Chris: That may be a judgement… [laughter] With our inaugural episode we figured we should probably start with the basics, and go over a few kind of key points here. Namely, I wanted to cover who works at the Northern New England Poison Center, what exactly is it that a poison center does, why should you call the poison center, and how do you get in contact with a poison center. So without further ado, Carolyn would you like to take it away and talk about who works here?
Carolyn: Sure, Chris. Most of the people who work here are nurses and pharmacists. Everybody is pretty much trained in health care, but more importantly we are specialists and uniquely trained in poison information and poison emergencies.
Karlee: Yes, and we are here all the time, 24/7…
Chris: 365…
Karlee: Yes, exactly. And, we take calls from the general public and various healthcare professionals, whether it be an emergency department or primary care office. We cover Maine, Vermont and New Hampshire.
Chris: Thus, Northern New England Poison Center. We’re one of 55 accredited poison centers across the United States. So, that’s just kind of a brief overview of who works is here, but we do want to cover what exactly the Northern New England Poison Center does. So Carolyn, do you want to expand on that?
Carolyn: Sure, before I talk about what a poison center does, let’s talk a little bit about what is a poison. Most people don’t really realize what the poison is, or what does it mean when you work at a poison center. A poison isn’t just a referring to a poisonous snake or a poisonous spider, ‘cause luckily we don’t really have many of those around here, if any.
Karlee: Yeah, that’s why I live here.
[laughter]
Carolyn: We appreciate that! But, a poison is anything that can cause harm. Whether it means it gets on your skin and causes a rash, or because you inhale it, or swallow it, or get it in the eye.
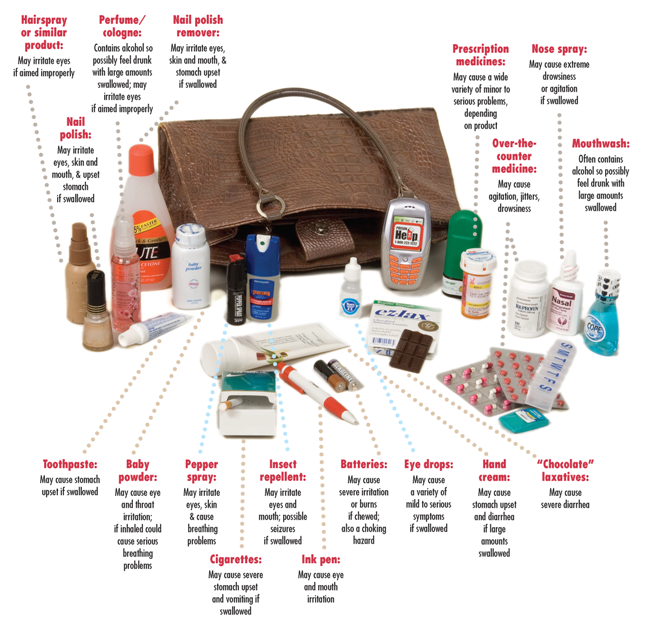
So, we deal with all of those, we don’t just deal with things that people swallow that they’re not supposed to, although that’s more common. We can tell you, for example, how to flush an eye over the phone. And we deal with poisons whether they are from around the home, or whether they’re in the workplace, or a medication error, or whether it’s something from the environment—any of those things! And you know, people often think that we just deal with children. We really don’t, we deal with anybody. You know, if you double dose your med by accident we’re going to be able to help you with that, or any of that kind of information.
Chris: If you are wondering if we can help, just call and we will always try our best to. You know, Karlee I think we should bring up, does it have to be an emergency for the public to reach out to us?
Karlee: No, good point. It doesn’t have to be an emergency and it doesn’t even have to be an exposure. We like to promote prevention here obviously, so you know if you’re thinking about maybe bringing something into an environment where there’s an individual who could be exposed. For example, you know you’re buying a new house plant and you have kiddos around. We can give you some toxicity information in general about the plant, and you can kind of use that to make decisions.
Chris: I think a lot of familiarity with poison centers just extends from getting a product and looking on the back and seeing that label that says “If swallowed, call the poison center, or 1-800-222-1222.” There isn’t as much familiarity with what exactly it’s like to call a poison center so, do we kind of want to go into what that experience is like?
Karlee: Yeah! It’s not just you know, you call us and we say and “That’s probably poisonous. Bye!”
[Laughter]
Carolyn: That would make our job a lot easier!
[Laughter]
Karlee: No, we really do a lot more for you than that. We will assess the situation, that’s what we’re trained for. We’ll triage to determine if you can be managed at home or if you do need to go into a health care facility.
Chris: Yeah, going along with that we should probably get into why we feel it’s important the community is aware of us, and why exactly they should call us. So do we kind of want to go into that as well?
Carolyn: Sure, so first of all, when you call the poison center, the person you are speaking with, the person who answers the phone, is the person who can help you. You don’t have to wait, it’s very quick. It’s one-on-one service and we’re not managing five other calls at the same time.
We’re talking to you and we’re going to deal with your emergency or your question. So it’s one-on-one, it’s quick, it’s confidential, judgement-free—we really are there to help.
Karlee: Yep, and aside from just good quality care, other perks are that we can save you time and money. So the time aspect, I mean that we get a lot of calls from people who say that they’ve been researching something for upwards of 30 minutes to an hour online and can’t really find anything. Well, we do have evidenced-based sources to kind of give you accurate and timely information.
Carolyn: Right. A lot of times when you look on the internet you see the worst case scenario. It doesn’t take into account how much, how old is the person, you know what exactly happened, and we can access all that, and we can do it very quickly.
Chris: Along with time we even have situations where people are worried that they need to run into the emergency department for something that’s, you know, not as much of an issue from our perspective. And we’re happy to let you know that, so—saves time, saves money.
Carolyn: Right, absolutely.
Chris: A fun fact that we like to say here is that for every dollar invested in a poison center saves $13 on the healthcare system. So, pretty good return on investment.
Carolyn: It’s pretty significant.
Chris: Carolyn also brought up one-on-one personalized care. We will follow up with you on the phone. We handle about 30,000 calls here yearly at the Northern New England Poison Center, and 9 out of 10 are just managed over the phone.
Carolyn: Right! We can save you that trip to the doctor or the emergency room. And we can let you—we will tell you if you need to go.
Karlee: Yep.
Chris: Right. I think the most important thing we could go over in this introductory episode however, is how exactly the communities we serve can get in contact with us. So, what’s the most common way?
Karlee: The most common is right over the phone, people calling us. So get out your pens, and write it down. The number is 1-800-222-1222. That is the national number but if you are in Maine, Vermont, or New Hampshire you’ll be routed to us. And you know if you call us, we will send you a magnet—stick it on your fridge.
Chris: We have pill reminder boxes too.
Carolyn: Lots of good stuff!
Chris: How about for the more tech savvy members of our community?
Carolyn: Sure, let me just mention that if you call we do have an interpreter service available as well, just so you know that. But you know, if you’d rather chat, you can chat through our website at nnepc.org, as in Northern New England Poison Center.org. Or, you can text POISON to 85511.
Chris: Well that’s the majority of, really, what we wanted to cover here in this introductory episode. But you know we do plan to have a lot in store, and we’re hoping to release episodes regularly. Any ideas on those topics we should be covering soon?
Karlee: Yeah we’re excited to expand on lots of different things. I think, you know, seasonal—sort of summer or fall, or even around the holidays, just certain things you should be aware of.
Carolyn: Yeah I mean we can do things like—we could do a whole podcast on mushrooms and berries, or carbon monoxide, or what children tend to get into and how to deal with that, so, we have a lot of ideas.
Chris: Yeah, so, plenty of material to work from, but we do want to say thanks again for listening to the first episode of Poison Center Pointers.
Carolyn: Yeah, thanks everybody!
Karlee: Thanks!
Chris: You can like, share, and subscribe to us on Facebook and Twitter, and again visit our website at nnepc.org, and if you have feedback or topics you’d like us to cover you can certainly send it to us.
Carolyn: Yeah, that’d be great.
Chris: But remember if you have an actual poisoning emergency, scenario, or even just a question contact the Northern New England Poison Center by calling 1-800-222-1222, text the word POISON to 85511, or chat online at nnepc.org. So, on behalf of Karlee, Carolyn and I, thank you so much for joining us today.
♪upbeat music♪