Many people who call the poison center are understandably worried, but the good news is nearly 9 out of every 10 calls from home can be safely managed with fast, expert help from our poison specialists, without needing to go to the hospital or doctor’s office.
 When you get on the phone with a poison specialist, there are a few things they will want to know to help you:
When you get on the phone with a poison specialist, there are a few things they will want to know to help you:
- How old is the patient?
- About how much does the patient weigh?
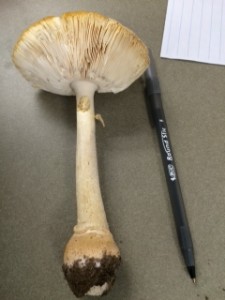
- What is the name of the product or substance involved? Be as specific as you can—it can help to have the bottle or packaging with you on the phone. Poison experts use a database that contains detailed information on thousands of products.
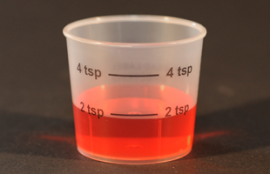
- How much of the substance did the patient swallow, breathe in or get on their skin? If you don’t know, the poison specialist will help you estimate.
Based on this information, the poison specialist will tell you what you need to do. It could be as simple as drinking some water or eating a popsicle. In rare circumstances, they may need to send you to the hospital. If so, they will ask which hospital you are closest to and call ahead to let them know you are coming.
You may be placed on hold at some point during your call to the poison center. Don’t worry—the poison specialist will be right back with you.
The poison center will also collect a little bit of personal information from you for your medical chart—your first name, the patient’s first name, your phone number and the zip code you are calling from. This information is confidential. This information is important because it helps us to find your case if you ever need to call about it again for any reason.